
What happens if you have an Ectopic Pregnancy?
Risk factors, symptoms, Types, Diagnosis, and Treatment of ectopic pregnancy
What is an Ectopic Pregnancy?
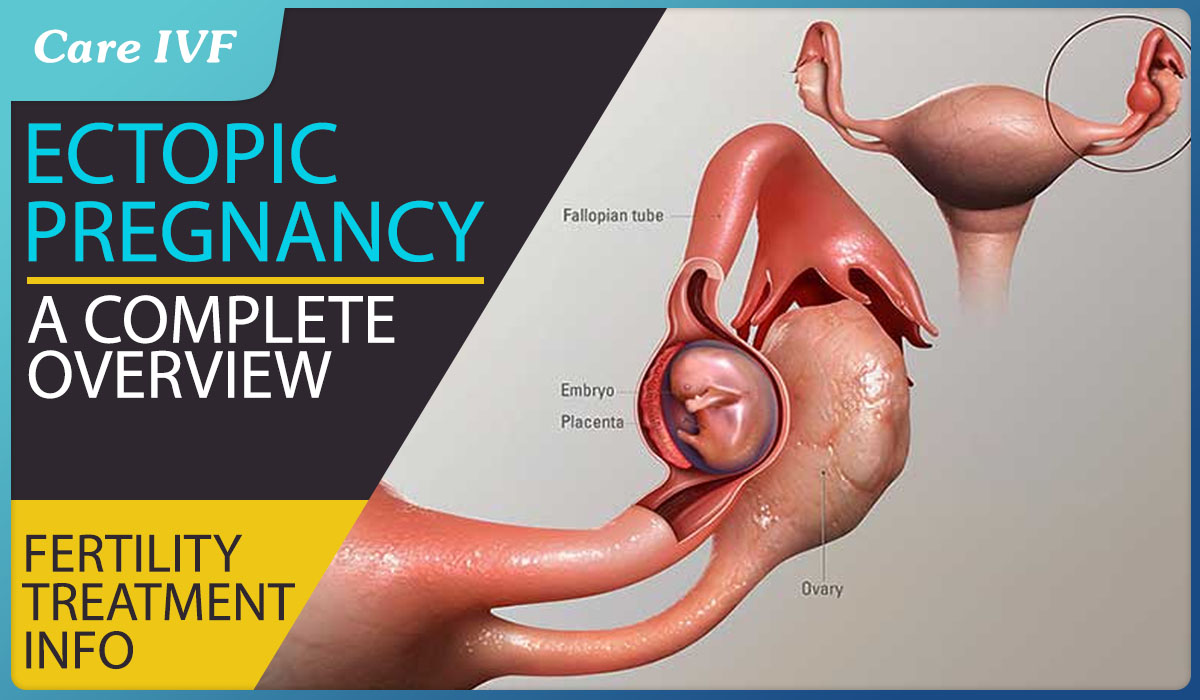
When the fertilized egg implants anywhere except the uterine lining, it is called an ectopic pregnancy. About one in 50 pregnancies are ectopic. Fallopian tubes are the most common part of the uterus where ectopic pregnancies occur and it accounts for almost 95%.
The movement of the fertilized egg from the fallopian tube to the uterus where it implants takes about 4 days and facilitated by tiny hair-like projections called cilia in the lining of the tubes.
Sometimes this transportation can be hampered by various reasons like scars/ damage to the tubes/adhesions/blocks and sometimes for no identifiable reason as well and this results in the implantation of the embryo in the tube.
Based on the location of Implantation ectopic pregnancy are of following types:
How soon would you know if you have an ectopic pregnancy?
Ectopic pregnancy may be asymptomatic in 9% of cases or it may present with:
- Amenorrhea (absence of menstruation)
- Abdominal pain
- Vaginal bleeding
Usually these symptoms appear within 6-8 weeks of a missed period.
What happens if an ectopic pregnancy keeps growing?
If an ectopic pregnancy keeps growing it will most likely rupture and case heavy bleeding and damage to fallopian tubes. it can also lead to removal of the damaged tubes.
Can ectopic pregnancy resolve by itself?
Approximately 40% of ectopic pregnancies can resolve on their own and require no further treatment. So watching and waiting is a viable option for enraptured ectopic pregnancies. In such a case the women are kept under observation for a day or two, if the beta hCG levels decline by 15% per day the woman can be sent home with no further treatment.
Are some women at a higher risk for ectopic pregnancy?
It has been seen that some Factors increases the risk of Ectopic Pregnancy in women:
- Pelvic inflammatory disease: Previous infection of the pelvic region, commonly chlamydia and gonorrhea, can sometimes damage the fallopian tubes. Chlamydia trachomatis attributes to 30-50% of all ectopic pregnancies.
- Smoking amongst women: Smoking can hinder the transfer of the ovum to the uterus by decreasing the ability of the muscles in the fallopian tube walls to contract.
- Prior pelvic or abdominal surgery: An embryo can implant in the scar tissue of the uterus lining, caused by a previous surgery
- History of pelvic infections: Infection and inflammation can damage the lining of the tube and cause scarring that can prevent the embryo from passing to the uterus
- Increased use of assisted reproductive technology (ART): This is due to Excessive Ovarian response, in cases of Endometriosis, mechanical factor infertility and previous Caesarean section
- Infertility: Women with infertility have a two or three times higher risk of ectopic pregnancy, possibly reflecting the increased number of people in this group who have tubal abnormalities, which may also be a cause of infertility.
- Age: Most ectopic pregnancies occur in women between the ages of 35 to 44.
Did you know: Women with a past history of ectopic pregnancy have more chances of ectopic pregnancies in subsequent conception? The increase in risk is directly proportional to the number of previous ectopic pregnancies
How to diagnose an Ectopic Pregnancy?
Ectopic pregnancies can be mostly diagnosed between 6 weeks’ and 10 weeks’ gestation.
Ruptured ectopic pregnancy may present with signs of hemodynamic instability (low blood pressure, increased heart rate and respiratory distress) and syncope (temporary loss of consciousness).
Visualization of a gestational sac outside the uterus, with yolk sac and/or fetal node with or without cardiac activity on transvaginal ultrasound (TVS) is the definitive diagnosis of ectopic pregnancy.
Appearance of free fluid in the pouch of Douglas in TVS with adnexal mass suggests ruptured ectopic pregnancy
What are the treatment options for ectopic pregnancy?
An ectopic pregnancy can be life threatening if left untreated and normally requires medical or surgical intervention to remove it. However, in some cases, when it is diagnosed early, ectopic pregnancy may be monitored to see if it will resolve on its own.
Treatment options depend on: 12
- HCG levels
- How many weeks pregnant the affected person is
- Size and impact of the ectopic pregnancy as shown on an ultrasound
- Pain levels
- General health
- The options the hospital has available
Can ectopic pregnancy be managed without surgery?
Nowadays, a more conservative approach has been established by offering medical management by using Methotrexate (MTX) injections with equally good success rates. However It should be under supervision in selected patients, only if diagnosed at an early stage.
How to select patients for medical management?
- Hemodynamically stable
- Blood hCG levels less than 1,500 are preferred.
- Absent cardiac activity
- No intrauterine pregnancy on ultrasonography (USG) scan
- Patient willing for regular follow up
- No known sensitivity to MTX
What kind of Surgical Intervention is done for Ectopic Pregnancy?
Salpingectomy and salpingectomy are two laparoscopic surgeries used to treat some ectopic pregnancies. In these procedures, a small incision is made in the abdomen, near or in the navel. Next, your doctor uses a thin tube equipped with a camera lens and light (laparoscope) to view the tubal area.
In a salpingectomy, the ectopic pregnancy is removed and the tube left to heal on its own. In a salpingectomy, the ectopic pregnancy and the tube are both removed.
Indications for Surgical Treatment:
- Ruptured ectopic with hemoperitoneum (accumulation of blood in the space between the inner lining of the abdominal wall and the internal abdominal organs.)
- Hemodynamically unstable patient
- Large ectopic
- Coexisting pathology requiring surgery, e.g. ovarian cyst, hydrosalpinx (fluid filled uterine cavity)
- Contraindication to medical management ( sac > 4 cm or hCG > 5,000 IU)
- Contraindication to methotrexate- liver, kidney, hematological, immune disorder or respiratory disease.
- Failure of medical treatment
- Select cases of ectopic pregnancy at sites other than fallopian tubes
Choice of Surgery:
The choice is based on tubal status and the age and parity of the woman.Salpingectomy:
- If the tube is ruptured already and the other tube looks healthy, the standard treatment is salphingectomy. Usually patient undergoing salphingectomy is relatively older.
- Salphingectomy may be partial or total depending on the patient’s age, site of ectopic, condition of tube and plan for future pregnancy.
- Laparoscopic salphingectomy may be carried out (removal of the affected tube)
Salpingostomy
- Salpingostomy is preferred if future childbearing is desired and the other tube is absent or damaged.
- A longitudinal incision is made over the gestation sac with cautery and products are evacuated and collected for pathological examination.
- Women undergoing salpingostomy should be followed up with hCG level
Effects of Ectopic Pregnancy management on Future Fertility:
- Long term studies have shown recurrent ectopic rate to be 18.5%
- Patency rates seen by hysterosalpingogram (HSG) were found to be similar in women who were managed medically or expectantly in either ipsilateral tube or in the contralateral tube.
- No adverse effect has been seen on the ovarian reserve of the patients after receiving the MTX.
- The oocyte recovery might be lower if fertility treatment is started within 180 days of giving MTX, so patients may be advised to use some kind of contraception and not plan pregnancy till 180 days of MTX.
- Conception should be avoided for at least 3 months after MTX administration as the drug remains in the system and can affect fetal development and can cause congenital malformations.
To conclude …
- Most ectopic pregnancies, even in the presence of hemperitoneum, may be treated with minimal invasive surgery, however, with acute bleeding, some surgeons prefer laparotomy.
- The crux is early diagnosis
Article Tags
About the author

Leave a Comment