
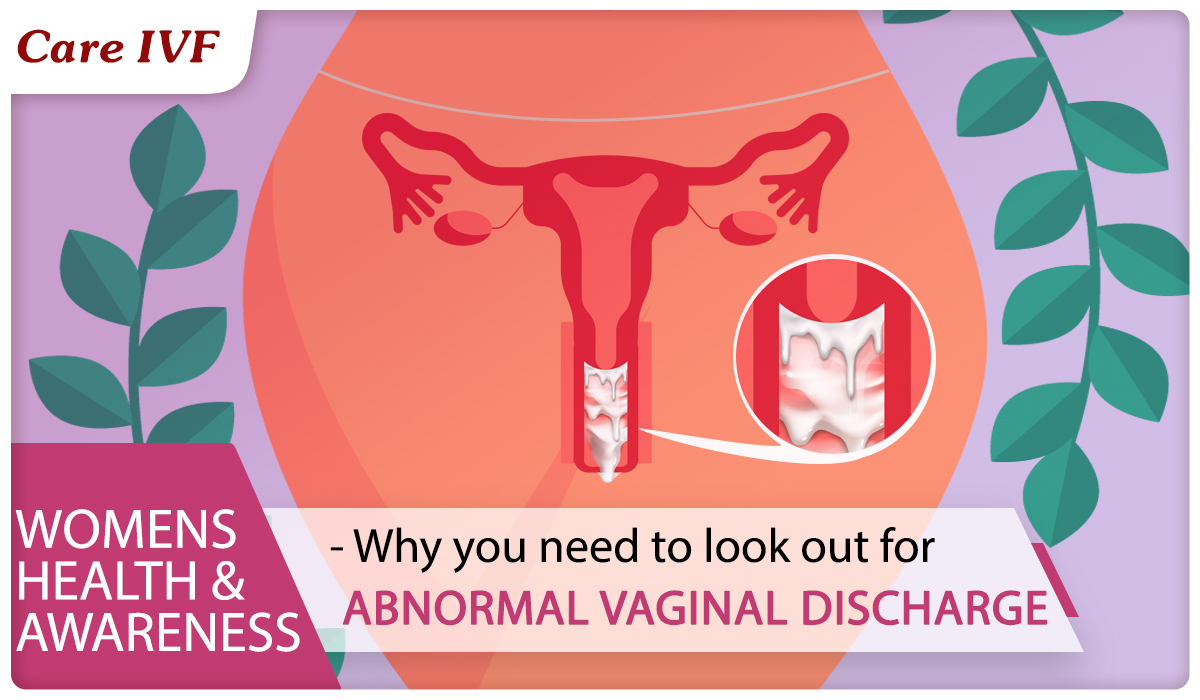
Are you having Vaginal Discharge? Here's what you must know
Vaginal discharge is normal – most women and girls get it. It's a fluid or mucus that keeps the vagina clean and moist, and protects it from infection.
Check if your vaginal discharge is normal
Vaginal discharge usually isn't anything to worry about if it: doesn't have a strong or unpleasant smell
- is clear or white
- is thick and sticky
- is slippery and wet
You can get vaginal discharge at any age.
The amount of discharge varies. You usually get heavier discharge during pregnancy, if you're sexually active or if you're using birth control. It's often slippery and wet for a few days between your periods (when you ovulate).
When it can be a sign of an infection
If your discharge changes – for example, in smell, colour or texture – it might be a sign of an infection. Possible causes for vaginal discharge may be:
| Type of Discharge | Possible cause |
| Smells fishy | Bacterial Vaginosis |
| Thick and white, like cottage cheese | Thrush |
| Green, yellow or frothy | Trichomoniasis |
| With pelvic pain or bleeding | Chlamydia or Gonorrhoea |
| With blisters or sores | Genital herpes |
The most common cause of pathological vaginal discharge in women of childbearing age is bacterial vaginosis.
Non-urgent advice: See your doctor if:
- your discharge changes colour, smell or texture
- you produce more discharge than usual
- you feel itchy or sore
- you bleed between periods or after sex
- you get pain when peeing
- you get pain in the area between your tummy and thighs (pelvic pain)
Types of Vaginal Discharge Presentations :
Infective (non-sexually transmitted) vaginal discharge
BV: Causes a thin, profuse and fishy-smelling discharge without itch or soreness.
Candidiasis: Thick, typically curd like, white, non-offensive discharge which is associated with vulval itch and soreness.
May cause mild dyspareunia and dysuria.
Infective (STI) vaginal discharge
Trachomatis, N. gonorrhoeae, and T. vaginalis can present with vaginal discharge but may also be asymptomatic. They are associated with an increased risk of HIV transmission.
- Chlamydia Trachomatis: May cause a copious purulent vaginal discharge but it is asymptomatic in 80% of women.
- Trichomonas Vaginalis: May cause an offensive yellow vaginal discharge, which is often profuse and frothy, associated with vulval itch and soreness, dysuria, abdominal pain and superficial pain during intercourse.
- Neisseria Gonorrhoeae: May present with a purulent vaginal discharge but is asymptomatic in up to 50% of women.
- Non-infective causes of vaginal discharge :
Retained foreign bodies - result in a foul-smelling discharge. Diagnosis is confirmed on examination.
Cervical polyps and ectopy - tend to be asymptomatic but there may be increased discharge and intermenstrual bleeding. Diagnosis is made on speculum examination.
Genital tract malignancy - presentation varies and, in some cases, a persistent vaginal discharge not responding to conventional treatment may be the first clue. Diagnosis is made on examination and biopsy.
Fistulae - history of trauma or surgery is suggestive. There may be a foul or feculent discharge in association with recurrent urinary tract infections.
Allergic reactions - diagnosis is suspected on taking the history - eg, use of irritant chemicals in douching, contact with latex and semen.
Vulval lichen planus and vulval dermatitis - will be apparent on examination but may require a skin biopsy to confirm the diagnosis.
Treatment for Vaginal Discharge depends upon cause.
Infective causes require dose of antimicrobials, depending upon the type suspected.
Management of persistent discharge:
In some cases, repeated examination and screening yield no positive results, yet the patient still complains of vaginal discharge.
It is then appropriate to explore with the patient the nature of the discharge and relate this to normal physiological discharge, to review personal hygiene habits (advise to avoid douches, perfumed products and tight synthetic clothing) and to explore the possibility of the hidden complaint, such as depression, anxiety or psychosexual dysfunction.
Postmenopausal atrophic changes may predispose women to repeated episodes of vaginitis which may respond well to hormonal creams or pessaries.
Complications of Untreated Vaginal Discharge?
Untreated, some vaginal infections can spread to the upper reproductive tract and cause more serious illness (pelvic inflammatory disease) and, in the long term, infertility.
A retained foreign body has the potential of leading to severe infection.
Cervical polyps are generally harmless although may cause infertility if they grow very large. Rarely, they may undergo malignant change (0.1%). There are specific complications associated with infective discharge in pregnancy, as outlined above.
How to prevent Vaginal Discharge?
- Basic personal hygiene (cleanliness without the use of douches and perfumed chemical agents, including so-called 'feminine hygiene' products) with avoidance of tight, synthetic clothing.
- Emollients can be used as a soap substitute and moisturiser to prevent dryness and maintain the skin's natural barrier functions.
- Treatment of sexual partners, as appropriate.
- You can't prevent vaginal discharge
- Panty liners can help with heavy or excessive discharge or if you're worried about any smell.
- To help prevent irritation, soreness or dryness:
- Do’s :
- wash gently
- use water and an emollient, such as E45 cream, or plain soap
- Don’ts:
- do not use perfumed soaps or gels
- do not use deodorants or scented hygiene wipes
- do not douche
- Do’s :
Article Tags
About the author

Leave a Comment